For most Medicare patients in United States right now, Medicare pays for hospital stays on the basis of what are called Diagnostic Related Groups or DRGs. You get diagnosed with pneumonia, and your hospital gets payment to treat a typical case of pneumonia. Name the diagnosis, and the hospital will know what it gets paid. And if the hospital keeps you in the hospital for 10 days longer than the average pneumonia patient, it will lose money on your care. On the other hand, if the hospital discharges you from the hospital quickly, it still receives payment for your pneumonia care. Plus, physicians and clinics can charge Medicare for outpatient services to follow-up on your hospitalization.
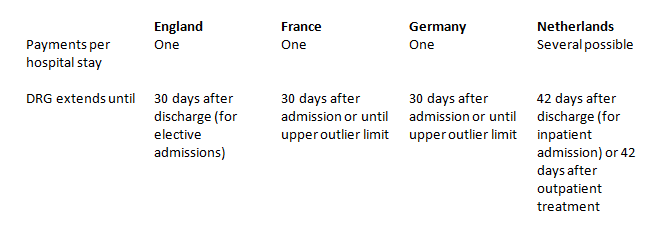
Under Obamacare, Medicare is going to start using more bundled payments, where the money the hospital receives for a diagnosis not only pays for the hospital care, but also for subsequent care after hospital discharge. Based on experience in Europe, this is a really good idea. As described in an April article in Health Affairs, the DRG systems in Europe are finer tuned than in the United States, promoting high quality of care while containing costs. One of the reasons is because the DRG extends beyond the hospital, as shown in the figure below: